Cutting-edge advancements from robotic surgery to targeted radiation beams are redefining cancer care. A new report highlights how precision-driven oncology is making treatments safer, more effective, and tailored to each patient’s needs. This shift promises a brighter future for cancer patients worldwide.
Precision Oncology’s Dual Approach of Robots and Radiation
Modern oncology now harnesses two powerful tools for precision healing:
- Robotic-assisted surgery: Using robotic systems gives surgeons enhanced dexterity and control. Instruments mimic human “wrist-like” movements with high precision. This allows minimally invasive tumour removal with less trauma, faster recovery, and reduced risk to surrounding healthy tissue.
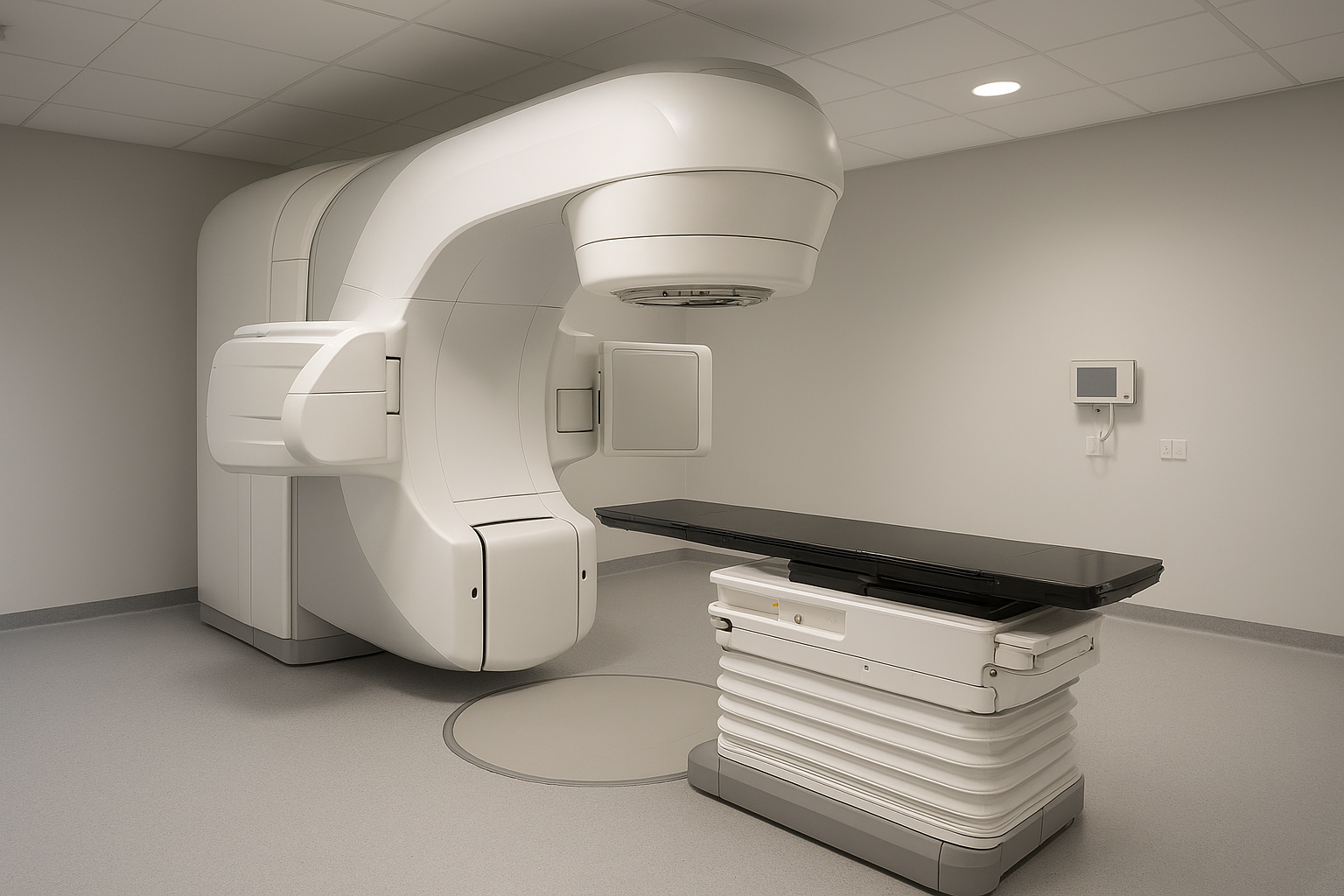
- Advanced radiation techniques: Radiation beams today are delivered with sub-millimetre accuracy, targeting tumours from multiple angles while sparing healthy organs. This is possible thanks to real-time imaging, motion tracking, and adaptive dose delivery.
Together, these methods offer a comprehensive “precision healing” model giving oncologists flexibility to choose the best approach depending on tumour type, location, and patient condition.
Why Oncologists Are Embracing Precision Healing
Oncology experts argue that the key advantage of robotic and high-precision radiotherapy lies in reducing collateral damage while maximizing treatment efficiency.
Robotic instruments provide “enhanced visualization, superior control, and minimal invasiveness,” which significantly lowers complications and improves post-surgery recovery.
On the radiotherapy front, techniques such as image-guided and intensity-modulated radiation therapy (IMRT), along with real-time imaging and adaptive planning, help deliver the exact radiation dose the tumour needs while limiting exposure to surrounding healthy tissue.
This dual approach allows treatment to be customized sometimes combining surgery and radiotherapy to maximize success and minimize side effects.
A Game-Changer for Cancer Care
The adoption of precision healing technologies represents a major leap forward for cancer treatment especially in complex or sensitive cases. Some of the benefits:
- Fewer complications and faster recovery after surgery due to minimally invasive robotic procedures
- Better quality of life, as healthy tissue and organs are preserved
- New treatment possibilities for tumours that are hard to reach or inoperable through conventional methods
- More personalized therapy plans tailored to tumour location, type, and patient physiology
Overall, “precision healing” not only improves clinical outcomes but also reduces patient suffering, side effects, and recovery time making cancer care more humane and effective.
The Future of Precision Oncology
Advancements likely to shape cancer care soon:
- Wider adoption of robotic-assisted tumour surgeries across hospitals, even for complex cancers.
- Growth of image-guided and adaptive radiotherapy (e.g. IGRT, IMRT, stereotactic radiotherapy) for more accurate, less invasive treatment.
- Integration of AI and data-driven planning to further personalize therapy optimizing radiation dose, tracking tumor motion, and predicting outcomes.
- Broader access to these technologies globally, bringing high-precision cancer care within reach for more patients.
Conclusion
Precision healing combining robotic surgery with advanced radiation therapy is transforming how we treat cancer. By targeting tumours with surgical finesse and beam accuracy, oncologists are achieving better outcomes, fewer side-effects, and personalized care. As these technologies become more accessible, the future of cancer treatment looks far more hopeful.